Something weird happened.
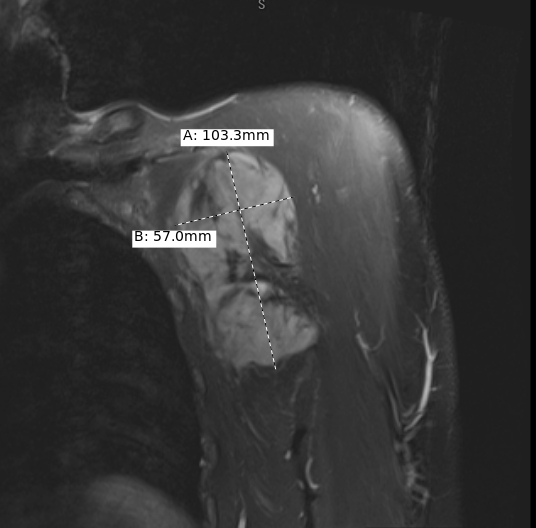 MRI of Left Axilla showing soft tissue mass
MRI of Left Axilla showing soft tissue mass
Seems rather large at 5.7cm X 10.3cm. Patient seemed unaware of the mass, but according to experts it probably had been growing there for years.
 See yellow arrow for location of left axilla
See yellow arrow for location of left axilla
From an accurate representation of the patient in question, The axilla is the name given to an area that lies underneath the glenohumeral joint, at the junction of the upper limb and the thorax. The more you know…
I GET A PIERCING AND A REAL TATTOO THIS YEAR!
Remember that tattoo I got in 2012 ?
Lookie HERE for details on that. Anyhow, this just goes to show what kind of trouble I get into. But it was not a real tattoo and since there are at least 22 tattoo places in town that also do piercing it still does not mean that I will get either (for various reasons we won’t go into at this time).
Now comes this Summer and it appears I do indeed get a piercing AND a tattoo and believe it or not, my insurance pays for it. Here’s how it went:
THE PIERCING:
So, the GP finds a bump on my arm and orders an ultrasound of the area in question. The report came back as a 6.1 x 9.9 cm left axillary mass concerning for malignancy. Differential diagnosis is lymphoma, metastatic adenopathy or possibly sarcoma. Recommend biopsy for diagnosis.
OK. nothing to see here. How about a CT scan. It confirms the following: Bones/soft tissues: Large left axillary mass measures 6.1 x 9.9 cm highly concerning for malignancy. Differential diagnosis is lymphoma, metastatic adenopathy or sarcoma. Recommend biopsy for diagnosis.
Seems redundant but what the hell. So a needle biopsy is ordered. Get it? A NEEDLE BIOPSY. That’s a piercing of the skin, so there you have it.
The pathology report on the sample taken was that it consisted of “a rubbery pink-gray-white, fibrofatty soft tissue without orientation.” Sounds about right. And under a microscope the sample was made up of spindle cells which according to Google are a narrow, elongated cell indicating the presence of a type of sarcoma. A second biopsy and/or pathology report from a fancy doctor in Boston says it’s a desmoid fibromatosis. I have a desmoid tumor!
OK, now what?
It’s off to a special surgeon in Denver at a place called The Institute for Limb Preservation because the location of the desmoid is between a rock and a hard place. Everybody said it would be difficult to remove surgically and even the Limb Preservation folks were not going to touch it (OK, the head surgeon did actually touch it and charged $480 to do so) so this thing may need chemo or radiation therapy.
After some research on some of the medical oncologists in Denver (even one described as ‘world famous’) and in town, it appeared that the direction I should take was to get zapped with radiation for five weeks and see what happens.
NOW COMES THE TATTOO:
In order to make sure the radiation reaches the tumor and not the nicer parts of the body, the radiation therapists create a molded pillow to keep the arm in place and then mark off areas for the radiation to pass using some quick CT scans of the area and program a set of laser guided sections to temporarily mark the path of the radiation. As a tertiary measure the therapists also permanently mark the skin with a TATTOO. They are very small dots and are hard to find, but they are REAL !
So that’s it. A piercing and a tattoo!
THE VARIAN TRUE BEAM AND 6DOF ‘PERFECT PITCH’ COUCH
Off to radiation oncology for 28 visits over a five and a half week period. I am lucky because the medical linear accelerator required for my radiotherapy is a relatively short distance from my home so I could ride my bike to treatment each morning. The accelerator in this case is a Varian Truebeam system utilizing high-precision Stereotactic Radiosurgery with HyperArc™– improved soft-tissue visualization via iterative Cone-Beam CT. Also, our little town’s oncology lab features the optional ‘Perfect Pitch’ six degree of freedom couch advanced robotics for accurate patient setup. (According to the Harmony Campus’ website, this is the ONLY Perfect Pitch couch in all of Colorado!)
Of course I got to meet other patients who came in for therapy– many of whom came from Wyoming and Nebraska traveling an hour and a half EACH DAY to get Radio. Therapy. Then. Drive. Back. Home. I wish them well.
As for me, never having experienced anything medical over an extended period of time, I thought it would be fun to create a little video of the RadioTherapy experience. Here it is below. It’s five and a half weeks reduced to six minutes. It’s a bit redundant but that’s what you would expect when you come in everyday for the same thing 28 times. The 56 Shades of Gray refers to the amount of radiation received from the accelerator using the unit of measure the Gray abbreviated Gy. In the video the numbers shown on the lower left indicate the absorbed radiation and each treatment came to 2.0 Gray per day.
56 Shades of Gray RadioTherapy Video
The music background in the video is ‘Desmoidian Rhapsody #6’ from a jam session I recorded a few years ago where I play a banjo. While making this video I imagined certain things while on the Perfect Pitch couch and I experimented with the editing effects in Kdenlive, the name of the video editing program I was using. The hardest part in making this video was getting the absorbed radiation counter to operate correctly.
Getting Weirder Still
Makerspace users like to see what they can get from certain types of data. I am a makerspace user and have my DICOM data from CT and MRI scans so why shouldn’t I make a model of this thing? Could I convert the MRI data into a single STL file and make a 3D print of the tumor?
There are a few programs for converting DICOM data into 3D printable files. I have seen many good models from biological specimens. Most are made from the scans of bones. We at the hub even have a member who specializes in biomedical engineering doing 3-D visualization and prototype development from DICOM data. But this tumor is not bone; it is not a functional structure and has many nooks and crannies because it is just there– a rapid fibromitosis that grows for no reason.
After looking at the individual sections it would appear that many of the sections may have a problem for printing because of a condition known as ‘Overhang’ . Overhang may cause the model to sag or curl without the proper support structures in place. Also, the end result in my opinion may be overly complex. The idea here is to estimate a size and shape. To that end, and to make the job simpler, I chose to make individual slices from the MRI and artistically remove the nooks and crannies in order to have a smoothed out version of the slices. Then, from these slices, I could cut out a template of each slice and stack them together. The picture above shows a thin piece of plywood that was cut using the hub’s laser cutter. The thickness of the model was based on the DICOM slice data obtained from the file header information. The length and width dimensions were from the measurements made by the oncologist.
After gluing the plywood pieces together (The holes in the plywood were intentionally placed to tie the slices together) I covered the wood with an air-dried clay material.
Painted in the color first described by the pathologists report from the first biopsy, the thing now becomes even more incredible when it can be held in your hand. A tangible tumor; hard to believe this is inside me.
UPDATE: After one year, the tumor is smaller!




